The title of a new study released April 28 by the Ethics and Public Policy Center is one Catholics, following the church's moral teaching, would agree upon: "The Abortion Pill Harms Women."
"Direct abortion, that is to say, abortion willed either as an end or a means," states the Catechism of the Catholic Church, "is gravely contrary to the moral law."
But it is the second part of the EPPC study title -- "Insurance Data Reveals One in Ten Patients Experiences a Serious Adverse Event" -- that has come under recent public scrutiny, both Catholic and secular.
EPPC is a Washington-based think tank working, as its name implies, at the intersection of moral values and civic decision making.
EPPC's study says its findings -- publicized as "the largest-known study of the abortion pill" -- reveal "an adverse event rate 22 times higher than the FDA-approved drug label reports."
"Following a mifepristone abortion," it says, "10.93% of women experience sepsis, infection, hemorrhaging, or another serious or life-threatening adverse event. That is, over one in ten patients experience at least one serious adverse event."
Citing the "new data" of the EPPC study on May 14, Health and Human Services Secretary Robert F. Kennedy Jr. ordered a new FDA review of mifepristone.
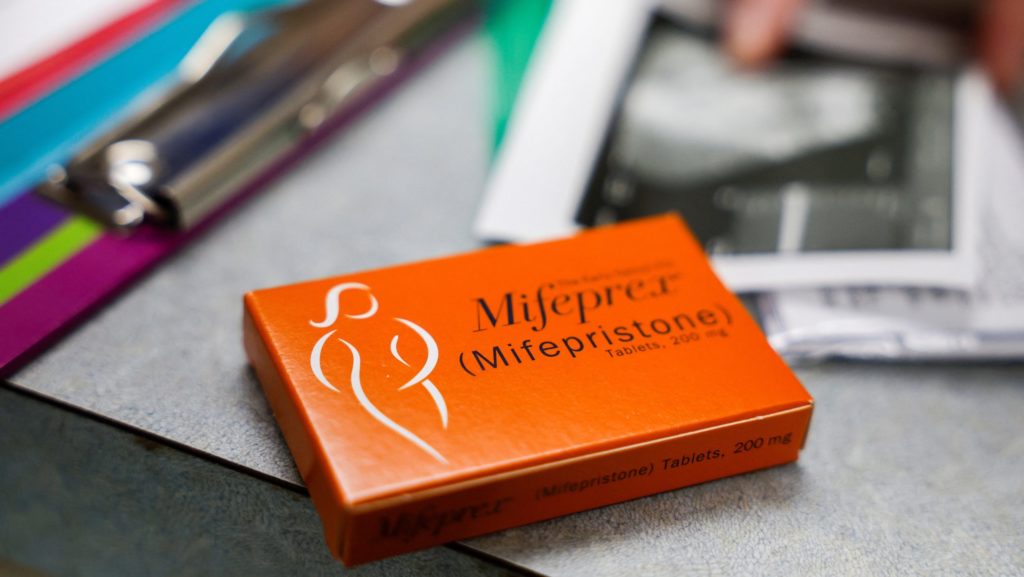
A synthetic steroid, mifepristone works by blocking the hormone progesterone, which is necessary for pregnancy to continue. When used in combination with misoprostol, which causes contractions, it can induce a "medication abortion." U.S. providers typically do not recommend the use of the two-step pill protocol for abortions beyond 10 weeks into a pregnancy.
According to the abortion research firm Guttmacher Institute, medication-based abortion accounted for 63% of all U.S. abortions in 2023 -- an increase from 53% in 2020.
Approved by the FDA for early abortion in 2000, mifepristone gained the moniker "the abortion pill" -- a designation that has become no longer accurate within the past decade.
Many OB-GYNs now use mifepristone and misoprostol together for early miscarriage care in order to more effectively expel any fetal remains and residual pregnancy tissue from the womb, and reduce the need for their surgical removal after the loss of a baby.
While misoprostol has been prescribed alone by OB-GYNs, the American College of Obstetricians and Gynecologists in recent years updated its protocols to recommend consideration of mifepristone and misoprostol in combination as more effective than misoprostol alone for early miscarriage care based on research published since 2018.
According to the National Library of Medicine, an estimated 26% of all pregnancies, and up to 10% of clinically recognized pregnancies, end in miscarriage, the loss of pregnancy less than 20-weeks gestation.
Which raises a serious and important question: If mifepristone is as dangerous as the EPPC study indicates, should women prescribed mifepristone for miscarriage care refuse to take it?
Because the Catholic Church teaches that all human life is sacred and must be respected from conception to natural death, it opposes the use of medicine when it is intended to cause direct abortion, which takes the life of the unborn child. However, the church also does not oppose the use of medicine when it is intended for restoring the body to health or life, which it calls "precious gifts entrusted to us by God."
"Many technologies and drugs have both moral and immoral uses," explained Father Tadeusz Pacholczyk, senior ethicist at the National Catholic Bioethics Center near Philadelphia.
"The abortion drug combination of mifepristone and misoprostol is frequently used in the immoral act of ending the life of an unborn child and expelling his or her remains from the mother's body," he said, "but the same two-drug regimen can also be used for the morally acceptable act of resolving a spontaneous miscarriage after the in utero child has died."
Father Pacholczyk illustrated with an example: "When there has been an incomplete miscarriage with only a partial expulsion of the pregnancy following embryonic or fetal death, there are no ethical objections to using the two-drug regimen of mifepristone and misoprostol to remove or expel the placental or other remaining tissues from the mother's body."
The use of mifepristone and misoprostol, said Father Pacholczyk, "parallels the use of other techniques like dilation and curettage (D&C) for either moral or immoral purposes."
"A D&C procedure may be used, in an immoral way, to carry out an abortion, bringing about the death and removal of a child from the mother's body," he said, "while the same technique can also be used in the aftermath of a spontaneous miscarriage, in a morally legitimate way, to remove fetal remains after a child has died in utero."
The Catholic Church unquestionably affirms -- as the EPPC study states -- that abortion harms women. But the church has also insisted on the development and evaluation of reliable data -- data that holds up to scrutiny both in the pro-life community and outside it -- in order to make the best arguments for life and avoid situations where the credibility of its teaching is undermined by tenuous or unreliable data.
OSV News asked doctoral-level faculty in both public health and research and evaluation programs at three Jesuit-run Catholic universities -- Boston College; Gonzaga University in Spokane, Washington; and Regis University in Denver -- to review and assess the methodological framework of the EPPC study.
The experts consulted included: Shaun Dougherty, program director for the research and evaluation methods, master of education, at Boston College's Lynch School of Education and Human Development; Robin Pickering, professor and chair of public health at Gonzaga University's School of Health Sciences; Martin Schiavenato, associate professor of nursing and public Health at Gonzaga University's School of Health Sciences; Andrea Bertotti Metoyer, professor of sociology and criminology at Gonzaga University; and Ksenia Polson, assistant professor in the Department of Marketing and Data Science at Regis University's Anderson College of Business and Computing.
Each of the reviewers raised concerns about the EPPC study as released April 28.
Polson remarked on "the absence of named researchers beyond the lead authors." She also noted that "the study highlights a percentage of adverse events following use of the abortion pill, but it only reports frequencies and percentages within a 45-day window. It does not provide statistical analyses -- such as correlations or randomized control trials -- that are necessary to establish causation or even strong associations."
Pickering observed that "there is no evidence that this research has undergone external scientific review, which is the standard for validating this type of research and to minimize bias. ... Without a formalized peer review process, the validity of the claims remains uncertain."
She added, "The author does not detail the full statistical methods used in the data analysis, which prevents accurate and complete critical analysis of methodological processes."
Schiavenato cautioned that "The combined use of multiple methods to define ‘adverse event' -- e.g., the FDA's FAERS system, CDC coding, CMS coding, and other ‘selective' coding performed by the authors -- without a clear explanation as to how this was done raises the possibility of counting an event multiple times."
"This very issue is acknowledged by the authors ... in terms of counting the same event multiple times in different categories," he said. "For this, too, the authors offer no explanation as to how the figures are adjusted."
The population sample assessed was also a perceived issue.
"It's difficult to verify whether the data are truly nationally representative in a way that would meet research standards," said Dougherty. "That is to say, they are not able to demonstrate that the characteristics of the people in the data look like a representative, or weighted and representative set of the population (or, in this case, female population of reproductive age)."
Another "challenging limitation" said Dougherty, "is that they are limited to individuals who make claims to their insurance to obtain and cover the cost of the medicine. The report does acknowledge that many women pay cash to obtain this medicine, and by extension this means that anyone not using insurance to cover these costs does not show up in the data."
Dougherty felt the EPPC report contained both accurate and ambiguous data.
"It is important to point out that while they are correct that it is important to understand how policies or in this case medication, plays out in common usage (not just controlled settings), it is potentially misleading to suggest, as the report does, that the data in the report are more representative than a clinical trial," he explained.
"By design, and law," added Dougherty, "published clinical trials have to conform to standards such that they can show that the group receiving a drug is statistically indistinguishable from the group who is not randomly assigned to receive it."
OSV News asked the Ethics and Public Policy Center to respond to a summary of the experts' analyses. EPPC responded by directing attention to two EPPC articles issued after the April 28 study: a May 6 fact sheet and a May 7 frequently asked questions document.
The fact sheet -- titled "Excluded Adverse Events in Real-World Study of Mifepristone" -- addressed the question of emergency room visits excluded from the study, while the FAQ document sought to clarify several points in light of the development that, as EPPC acknowledges, "some have raised questions about our data and methodology."
OSV News shared the two new EPPC documents with the previously consulted university researchers, to ask if they impacted their earlier assessments.
"While these documents complement or provide additional context on the report, none of them address the critiques that I shared," Dougherty replied. "The primary issue being the self-selection into using insurance to pay for the medication, which changes the population to which one might reasonably generalize, and does not account for the range of unobserved factors that would have been taken into account in the random-assignment clinical trials."
"My assessment of the study is the same," said Polson. "The study lacks statistical analysis to support the claims the authors are making."
"The 'answers' and explanations on these documents do not address the core of our combined critique -- that is, the lack of transparency on methodology and the missing peer-review process," Schiavenato observed.
He added that the peer-review process is designed to act as a "safety layer to ensure the validity, accuracy and overall scientific merit of the work before it is published."