When does the brain die? While the concept of brain death has been widely accepted by medical professionals since the late-1960s, significant questions about its precise nature still remain.
The National Catholic Bioethics Center (NCBC) released “Integrity in the Determination of Brain Death: Recent Challenges and Next Steps” to draw attention to recent events that should give rise to grave concerns and that call on Catholic leaders in the medical and health sectors to bring consistence and clarity on the issue.
There are two ways medical staff can declare someone dead. The most common is known as “circulatory death,” where a person’s heart stops beating and cannot be restarted.
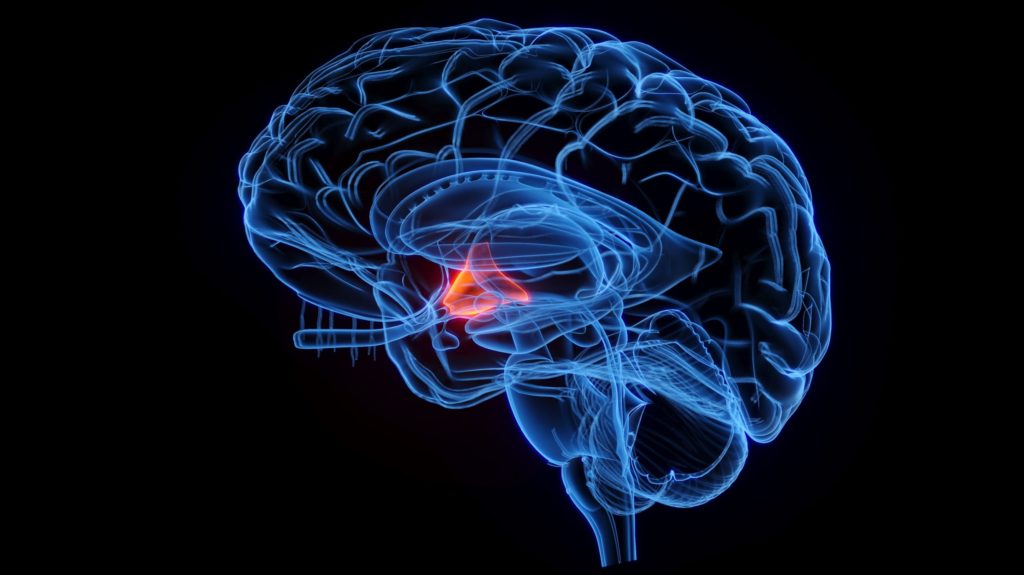
The second method is brain death. This is declared when a person has sustained catastrophic brain injury causing the permanent cessation of all brain function.
However, people who have suffered a “brain death” can still be breathing with support and have a heartbeat. This makes them better options for giving organ transplants, which has caused some doctors to want to modify the description of what causes brain death.
The NCDC says organ transplantation has extended the lives of thousands of people, but note the Church teaches that vital organs – including hearts, lungs, and livers – may only be taken after a patient is truly dead.
“The failure to resolve an important inconsistency between clinical, legal, and ethical standards for brain death has revealed an emerging breakdown in the public consensus on death and organ donation which, if not addressed, will undermine respect for the sanctity of human life and support for organ transplantation,” said John Brehany, the executive vice president and director of institutional relations at the NCBC.
“It is essential that Catholics in medicine, health care delivery, and academe help to bring clarity and consistency at this critical time,” he said.
The NCBC’s new document notes there have been questions and tensions surrounding the concept and determination of brain death for decades.
“In the context of academic articles, some have blatantly admitted that individuals pronounced dead by neurological criteria are not really dead. Others have pointed out multiple ambiguities inherent in brain death standards and then called for new standards that would permit taking vital organs from patients who are profoundly brain injured but not brain dead,” the document reads.
In an article for NPR’s Morning Edition, critics of the current definitions of “brain death” point to rare cases like Jahi McMath, a 13-year-old girl who was declared brain dead in 2013, but lived for years after her family refused to withdraw life support. She continued to grow and even went through puberty before she eventually died.
“I’ve never heard of a corpse that underwent puberty before,” Dr. D. Alan Shewmon, a professor emeritus of pediatrics and neurology at the David Geffen School of Medicine at the University of California, Los Angeles, told Morning Edition.
“She was clearly not dead. Yet she was declared dead. I think it’s a tragedy. How many others are potentially like that but we never find out?” Shewmon said.
Joseph Meaney, President of the NCBC said the main source of controversy has been a number of cases where individuals were misdiagnosed as brain dead and then clearly were still alive.
“This led to questions about how accurate clinical testing for brain death is and if enough neurological factors are being tested,” he told Crux.
“The main cause of concern at present in the United States is that while the law clearly requires irreversible cessation of all functions of the brain for a person to be declared dead using neurological criteria, the main protocol for clinical diagnosis of brain death pointedly does not assess neuroendocrine functioning in the patient’s brain,” Meaney said.
“If the hypothalamus in the brain is still functioning, then both legally and ethically – from a Catholic perspective – that person should not be declared brain dead. The NCBC and many others see the need for more comprehensive diagnostic testing to give the required moral certainty of death before the transplanting of vital organs is allowed,” he added.
The new document says beyond ensuring that the deaths of potential candidates for organ donation are determined with rigor and consistency, it will be important to examine how strengthened ethical standards and testing protocols will intersect with governmental regulations, clinical standards, and the significant financial reimbursements related to organ transplantation.
“This will not be easy. Yet, we cannot ignore or shrink from these tasks,” the document says.
Meaney told Crux that Pope John Paul II made a well-known address in August 2000 that said “the complete and irreversible cessation of all brain activity, if rigorously applied, does not seem to conflict with the essential elements of a sound anthropology.”
“Therefore, a health-worker professionally responsible for ascertaining death can use these criteria in each individual case as the basis for arriving at that degree of assurance in ethical judgement which moral teaching describes as ‘moral certainty’,” John Paul added.
“Pope Benedict XVI reinforced his predecessor’s statement, particularly when it comes to the grave responsibility to have certitude that the person has died prior to vital organ donation,” Meaney said.